Understanding Costochondritis - Separating Chest Pain from Heart Attack Symptoms
What is Costochondritis?
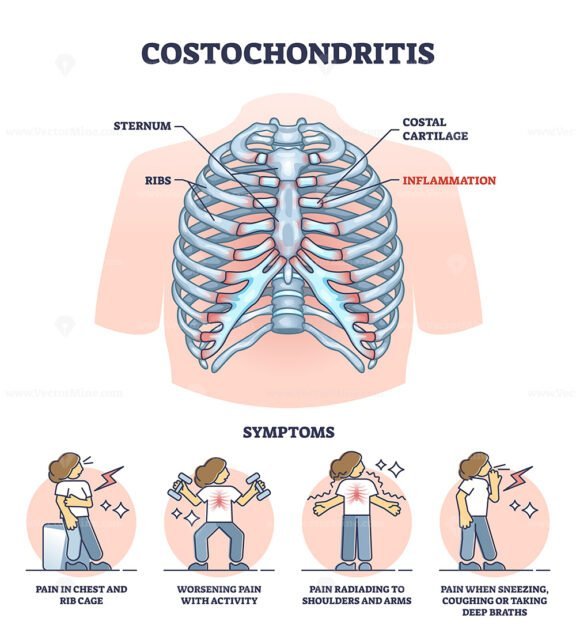
Costochondritis is a benign inflammation of one or more of the costal cartilages, connecting the ribs to the breastbone (sternum). This condition is also known as Chondrocostal Junction Syndrome or Tietze syndrome, classified under the ICD-10 code M94.0.
Understanding the Condition
Costochondritis primarily affects the upper ribs, especially on the left-hand side, causing chest wall pain. The inflammation occurs at the junction where the ribs meet the cartilage, leading to sharp or dull pains in the chest. While it can be unsettling, costochondritis is generally harmless and not indicative of a heart attack or other serious cardiac conditions.
Key Characteristics
- The pain is typically localized to the left side of the chest, near the breastbone.
- Pain can radiate to the shoulder or arm.
- Movement or deep breathing can exacerbate the discomfort.
- The condition often resolves on its own within a few weeks.
It's essential to note that while costochondritis is not directly related to heart health, its symptoms can be alarmingly similar to those experienced during a heart attack. If you're experiencing persistent or severe chest pain, it's crucial to seek medical attention to rule out any life-threatening conditions.
By understanding costochondritis and its characteristics, individuals can better identify their symptoms and seek appropriate medical evaluation and treatment, ensuring peace of mind and effective management of their condition.
Causes and Risk Factors
While the exact cause of costochondritis remains unclear, researchers have identified several potential triggers and risk factors that contribute to its development.
Potential Triggers
Several factors can potentially trigger costochondritis, including:
- Infection: Viral or bacterial infections, such as respiratory tract infections, may lead to costochondritis.
- Injury: Trauma to the chest wall, such as from a fall or car accident, can cause inflammation of the costochondral junction.
- Strain: Overuse or repetitive strain on the chest muscles, often from activities like heavy lifting, bending, or exercise, may contribute to costochondritis.
Risk Factors
Certain individuals are more likely to develop costochondritis due to the following risk factors:
- Family History: Having a family history of costochondritis may increase a person's likelihood of developing the condition.
- Gender: Costochondritis is more common in females than males.
- Age: Costochondritis typically affects adults between 40-50 years old, although it can occur at any age.
It's essential to note that costochondritis can affect anyone, regardless of age or sex. If you experience persistent or severe chest pain, consult a healthcare professional for proper diagnosis and treatment.
Symptoms and Diagnosis Understanding the symptoms and diagnostic process of costochondritis is crucial for effectively managing the condition and alleviating concerns about potential heart-related issues. Identifying Key Symptoms Costochondritis presents with distinct symptoms that can be alarming, especially for those unfamiliar with the condition. The primary symptoms include: Chest Pain: Dull to sharp pain at the front of the chest wall, radiating to the back or abdomen. This pain is typically localized to the area where the ribs meet the breastbone (sternum) or the cartilage that connects the ribs to the sternum. Movement-Related Pain: Pain worsens with movement or deep breathing, indicating inflammation of the costal cartilage. Localized Tenderness: Pressing on the affected area can reproduce the pain, confirming its origin. Diagnostic Process Diagnosing costochondritis involves ruling out life-threatening causes like heart attacks or coronary artery disease. Healthcare professionals employ a systematic approach: Medical History: A thorough review of the patient's medical history to identify potential risk factors or underlying conditions. Physical Examination: A careful examination to assess chest pain, movement-related pain, and localized tenderness. Diagnostic Tests: Tests such as electrocardiograms (ECGs), chest X-rays, or cardiac enzymes may be ordered to exclude cardiac causes. Differential Diagnosis: Considering other potential causes of chest pain, such as gastroesophageal reflux disease (GERD), pulmonary embolism, or musculoskeletal disorders. Importance of Accurate Diagnosis Accurately diagnosing costochondritis is essential for: Relief from Anxiety: Confirming that chest pain is not related to a life-threatening condition significantly reduces patient anxiety. Targeted Treatment: An accurate diagnosis allows for tailored treatment strategies focusing on managing inflammation and pain. Preventing Mismanagement: Avoids unnecessary cardiac interventions and ensures appropriate management of symptoms. By understanding the symptoms and diagnostic process of costochondritis, individuals can better navigate their healthcare needs and find effective relief from chest pain.
Treatment and Management
Costochondritis is typically managed with conservative treatments focused on alleviating symptoms, particularly chest pain. The primary objective is to reduce discomfort and improve quality of life.
Conservative Treatments
The following approaches are commonly employed to manage costochondritis:
- Rest and Ice: Avoiding activities that exacerbate the condition and applying ice to the affected area can help reduce pain and inflammation.
- Pain Medication: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can provide relief from pain and inflammation.
- Physical Therapy: Gentle exercises and stretches can help improve mobility and strength in the chest and shoulder muscles, reducing tension on the costosternal joints.
Further Medical Attention
In rare instances, costochondritis may be caused by an underlying condition that requires prompt medical attention. These include:
- Tumors: In rare cases, a tumor may be pressing on the costosternal joints, causing pain.
- Infections: Bacterial or fungal infections can affect the costosternal joints, requiring antibiotics or antifungal medication.
- Other underlying conditions: Certain conditions, such as rheumatoid arthritis or lupus, may contribute to costochondritis. Managing these underlying conditions can help alleviate symptoms.
It is essential to consult a healthcare professional for an accurate diagnosis and treatment plan, as costochondritis can mimic heart attack symptoms. A proper evaluation will determine the best course of treatment and rule out any underlying conditions that may require immediate attention.
Complications and Prognosis While costochondritis is generally a benign condition, it's essential to understand the potential complications and prognosis to ensure timely medical attention when necessary. Typical Outcome
Resolution Without Complications
In most cases, costochondritis resolves on its own within a few weeks to months without any significant complications. With proper rest, physical therapy, and pain management, patients can experience complete recovery. Rare But Potential Complications
Persistent Joint or Bone Damage
In rare instances, recurring or severe costochondritis episodes can lead to chronic joint or bone damage. This may result in: Chronic pain and stiffness Reduced mobility Increased risk of osteoarthritis
Tumor Spread (Extremely Rare)
Although extremely rare, it's crucial to note that costochondritis can, in very rare cases, be associated with underlying conditions such as: Tietze's syndrome (benign inflammation of the chest cartilage) Primary or metastatic tumors affecting the sternum or ribs In such cases, prompt medical evaluation is critical to rule out these rare but potentially serious conditions. Prognosis and Long-Term Outlook The prognosis for costochondritis is generally excellent, with most patients experiencing: Full recovery No long-term consequences No increased risk of heart disease or other cardiovascular conditions However, it's vital to maintain awareness of the symptoms and seek medical attention if they recur or worsen over time.Conclusion Costochondritis, a condition often masquerading as a heart attack, necessitates prompt medical evaluation to distinguish it from life-threatening cardiovascular emergencies. Fortunately, costochondritis is a treatable condition that requires medical attention primarily to rule out more severe causes. Understanding its symptoms and treatment options can alleviate concerns and promote effective management. Key Takeaways Accurate Diagnosis is Crucial: Distinguishing costochondritis from heart-related conditions is vital. A thorough medical evaluation ensures appropriate treatment and alleviates unnecessary anxiety. Treatable Condition: Costochondritis responds well to conservative treatments, including pain management, physical therapy, and lifestyle adjustments. Preventive Measures: Maintaining good posture, engaging in regular exercise, and avoiding heavy lifting can help prevent costochondritis. Open Communication: Patients should openly discuss symptoms and concerns with healthcare providers to ensure personalized care. Moving Forward By acknowledging the differences between costochondritis and heart attack symptoms, individuals can seek timely medical attention, facilitating accurate diagnoses and effective treatment plans. Raising awareness about costochondritis promotes better understanding and management of chest pain, ultimately enhancing overall well-being. Final Thoughts Costochondritis may mimic heart attack symptoms, but its treatable nature offers relief. Through education and awareness, we can empower individuals to navigate chest pain with confidence, ensuring that each ache is met with informed action rather than panic.











Comments ()