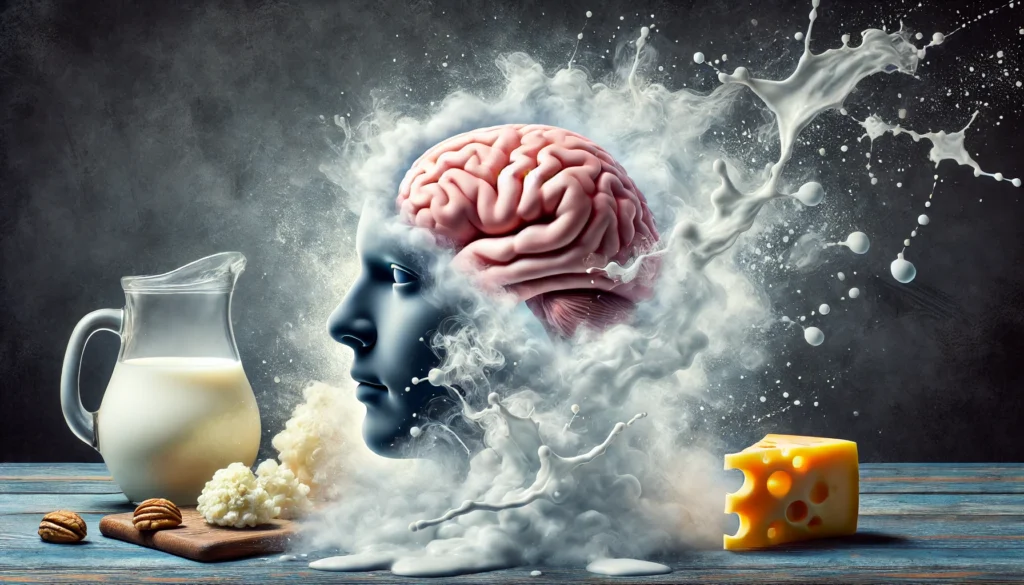
Silent Liver, Loud Risks - Fatty Liver Disease and its Impact on Brain Health

Often dubbed a "silent disease" due to its subtle onset, fatty liver disease (FLD) is steadily climbing the ranks of global health concerns. Affecting nearly 25% of the world's population, this condition, characterized by excessive fat accumulation in the liver, extends its reach far beyond the confines of the liver itself.
While the link between FLD and metabolic disorders like diabetes and heart disease is widely recognized, recent research is uncovering a more alarming connection - the impact of FLD on brain health. This article delves into the intricate relationship between fatty liver disease and brain health, highlighting the latest findings and emphasizing the importance of early detection and intervention.
Beyond Metabolism: Unraveling the Fatty Liver-Brain Axis
For years, FLD was primarily associated with metabolic dysfunction, leading to conditions like insulin resistance, type 2 diabetes, and cardiovascular disease. However, emerging evidence suggests a more complex picture, implicating FLD in a broader spectrum of health issues, including cognitive impairment and neurodegenerative diseases.
Central to this understanding is the gut-liver-brain axis, a complex communication network linking these three vital organs. In the context of FLD, this axis becomes disrupted, leading to systemic inflammation and oxidative stress that can negatively impact brain function.
Inflammation: The Common Culprit
Inflammation, the body's natural defense mechanism, plays a critical role in the pathogenesis of FLD. When fat accumulates in the liver, it triggers an inflammatory response, releasing inflammatory cytokines into the bloodstream. These inflammatory molecules can cross the blood-brain barrier, a protective shield surrounding the brain, disrupting normal neural activity and contributing to neuroinflammation.
Chronic neuroinflammation is increasingly recognized as a key player in the development of neurodegenerative diseases, such as Alzheimer's disease and Parkinson's disease. A 2022 study published in the journal "Nature Reviews Gastroenterology & Hepatology" highlighted the role of systemic inflammation originating from the liver in driving neuroinflammation and subsequent cognitive decline in individuals with FLD.
Oxidative Stress: Tipping the Balance in the Brain
Oxidative stress, an imbalance between the production of harmful free radicals and the body's ability to neutralize them, is another significant consequence of FLD with detrimental effects on the brain. The liver, a primary site for detoxification, becomes overwhelmed in the face of FLD, leading to increased production and reduced clearance of free radicals.
These highly reactive molecules can damage brain cells, impairing their function and increasing the risk of neurodegeneration. A study published in the journal "Hepatology" found that individuals with non-alcoholic fatty liver disease (NAFLD), the most common type of FLD, exhibited higher levels of oxidative stress markers in the brain compared to healthy controls. This oxidative damage was associated with poorer cognitive performance and an increased risk of cognitive decline.
Altered Brain Structure and Function: A Tangible Impact
The inflammatory and oxidative insults brought about by FLD can manifest as structural and functional changes in the brain. Studies utilizing advanced imaging techniques like magnetic resonance imaging (MRI) have revealed that individuals with FLD often exhibit reduced brain volume, particularly in areas crucial for memory, attention, and executive function.
Moreover, FLD is associated with impaired cerebral blood flow, reducing the delivery of oxygen and nutrients to brain cells. This compromised blood flow can further exacerbate cognitive impairment and accelerate the progression of neurodegenerative diseases.
From Fatty Liver to Cognitive Decline: A Growing Concern
The cumulative effects of inflammation, oxidative stress, and altered brain structure and function can significantly increase the risk of cognitive decline and dementia in individuals with FLD. A 2023 meta-analysis published in the journal "The Lancet Gastroenterology & Hepatology" analyzed data from over 2 million individuals and found that those with NAFLD had a 35% increased risk of developing dementia compared to those without the condition.
These findings underscore the critical need for early detection and management of FLD to mitigate its long-term impact on brain health. Addressing modifiable risk factors, such as obesity, insulin resistance, and unhealthy dietary habits, is paramount in preventing FLD progression and protecting brain function.
Protecting Your Brain: A Call to Action
The link between fatty liver disease and brain health is a burgeoning area of research, with new insights emerging regularly. While further studies are needed to fully elucidate the complex interplay between these two vital organs, existing evidence underscores the importance of a proactive approach to liver health.
Lifestyle modifications, including maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet rich in fruits, vegetables, and whole grains, are crucial for both preventing and managing FLD. Early detection through regular health checkups and appropriate medical intervention can help prevent the silent progression of FLD and its potentially devastating consequences on brain health.
Taking Charge of Your Health: One Step at a Time
The intricate connection between fatty liver disease and brain health highlights the interconnectedness of our body's systems. By prioritizing liver health, we are not only safeguarding this vital organ but also protecting our cognitive function and reducing the risk of neurodegenerative diseases.
Through increased awareness, proactive lifestyle choices, and timely medical intervention, we can mitigate the impact of FLD on brain health and pave the way for a healthier future.










Comments ()