Optimal Timing - Taking High Blood Pressure Meds at Bedtime

The Importance of Timing in Blood Pressure Medication
Unlocking the Secrets of Optimal Timing
When it comes to managing high blood pressure, timing is everything. Research has shown that taking blood pressure medication at bedtime may be more effective in reducing the risk of heart and blood vessel disease. But why is this the case, and what does it mean for individuals with hypertension?
The Daily Rhythm of Blood Pressure
Blood pressure follows a daily rhythm, peaking in the daytime and dipping at night. This natural fluctuation is known as the circadian rhythm. Typically, blood pressure drops by 10-20% at night, a phenomenon known as nocturnal dipping. However, in some individuals, this dipping does not occur, leading to increased cardiovascular risk.
Bedtime Medication: A Game-Changer?
Studies have shown that taking blood pressure medication at bedtime can help restore the natural nocturnal dipping pattern. This, in turn, can reduce the risk of heart and blood vessel disease, including conditions like myocardial infarction, stroke, and cardiac arrhythmias. Additionally, bedtime medication may also improve blood pressure control and reduce morning blood pressure surges.
Personalized Approach: Tailoring Medication Regimens
While bedtime medication may be beneficial for some, it's essential to remember that individual circumstances play a significant role. Experts recommend personalized medication regimens based on factors like lifestyle, sleep patterns, and medication type. For instance, individuals with kidney disease or sleep apnea may require alternative timing strategies.
Consult Your Doctor: The Key to Optimal Timing
In conclusion, the timing of blood pressure medication is a crucial aspect of hypertension management. While bedtime medication may be beneficial for some, it's essential to consult with your doctor to determine the best approach for your unique situation. By working together, you can unlock the secrets of optimal timing and take control of your blood pressure.
The Science Behind Bedtime Medication
When it comes to managing high blood pressure, timing is everything. Research has shown that taking medication at bedtime can have a significant impact on controlling blood pressure and reducing cardiovascular risk. But what's behind this optimal timing, and how does it align with our natural bodily rhythms?
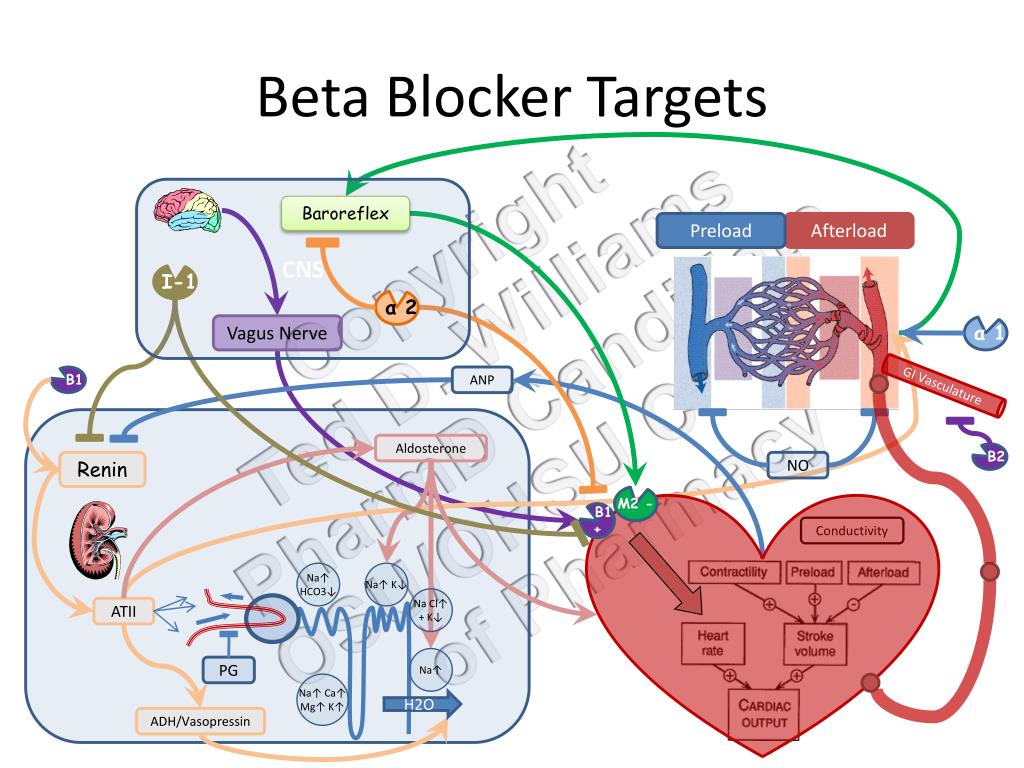
Chronotherapy: Aligning with the Body's Natural Clock
Chronotherapy, the study of the relationship between biological rhythms and medication timing, supports taking high blood pressure medication at bedtime. Our bodies have an internal clock that regulates various physiological processes, including blood pressure. By taking medication at bedtime, we can align with these natural rhythms to optimize treatment efficacy.
Nighttime Blood Pressure: A Critical Factor
Studies have consistently shown that nighttime blood pressure is often higher than morning blood pressure. This is because our bodies experience a natural dip in blood pressure during sleep, known as the "dipping phenomenon." However, individuals with high blood pressure often experience a non-dipping or reverse dipping pattern, where nighttime blood pressure remains elevated. Taking medication at bedtime helps regulate this nighttime blood pressure, reducing cardiovascular risk.
Regulating Nighttime Blood Pressure: The Benefits of Bedtime Medication
Taking high blood pressure medication at bedtime has been shown to:
- Reduce nighttime blood pressure and promote a healthier dipping pattern
- Decrease cardiovascular risk, including heart attacks, strokes, and kidney disease
- Improve blood pressure control and reduce morning blood pressure surges
- Enhance the effectiveness of medication, reducing the need for additional treatments
By synchronizing medication timing with our natural bodily rhythms, we can unlock the full potential of treatment and take control of our blood pressure. Consult with your healthcare provider to determine if bedtime medication is right for you.
Debunking the Morning Medication Myth For years, conventional wisdom dictated that individuals with hypertension take their blood pressure medication in the morning. However, recent research challenges this long-held assumption, suggesting that bedtime may be a more effective time for taking hypertension medication. The Traditional Approach: Morning Medication
The Rationale Behind Morning Medication
Traditionally, healthcare providers advised patients to take their blood pressure medication in the morning for several reasons:
Aligning medication schedules with daily routines Improving adherence and minimizing missed doses Reducing morning blood pressure surges The Shift to Bedtime Medication
Challenging the Status Quo: The Benefits of Bedtime Medication
Studies have revealed that taking blood pressure medication at bedtime may provide better blood pressure control and reduce cardiovascular risk. This is attributed to several factors:
Improved Nighttime Blood Pressure Regulation: Blood pressure naturally dips at night. Taking medication before bed helps maintain this natural dip, reducing cardiovascular strain. Enhanced Endothelial Function: Bedtime medication may improve endothelial function, which is critical for maintaining healthy blood vessels. Better Blood Pressure Control: Research indicates that bedtime medication schedules are associated with improved blood pressure control and reduced cardiovascular events. The Drawbacks of Morning Medication
The Limitations of Morning Medication
While morning medication may provide initial blood pressure control, it may not offer adequate protection throughout the night:
Insufficient Nighttime Coverage: Morning medication may wear off during the night, leaving individuals vulnerable to blood pressure spikes. Increased Cardiovascular Risk: Uncontrolled nighttime blood pressure is linked to increased cardiovascular risk, including heart attacks, strokes, and kidney damage. Conclusion Taking high blood pressure medication at bedtime may offer superior benefits compared to traditional morning schedules. Consult your healthcare provider to determine the optimal timing for your hypertension medication.
Consult Your Physician: Personalized Medication Plans
When it comes to taking high blood pressure medications, timing is crucial for optimal effectiveness. While research suggests that taking medications at bedtime may be beneficial for many individuals, it's essential to consult with your physician to determine the best approach for your unique circumstances.
Individual Circumstances Matter
Your lifestyle, medical history, and specific health needs can significantly influence the optimal timing of your medication. For instance:
- Lifestyle factors, such as work schedules, sleep patterns, and daily routines, can impact medication timing.
- Underlying medical conditions, like kidney disease or diabetes, may require adjusted medication schedules.
- Age and overall health can also affect medication absorption and effectiveness.
The Importance of Physician Guidance
Physicians play a vital role in helping patients develop personalized medication plans. Your doctor should discuss the following factors with you:
- Medication type and dosage
- Timing of medication in relation to meals and sleep
- Potential interactions with other medications
- Monitoring and adjusting medication plans as needed
Customized Medication Regimens
Medication regimens may vary significantly depending on specific health needs. Your physician may recommend:
- Once-daily medications for simplicity and adherence
- Twice-daily or multiple-daily medications for tighter blood pressure control
- Combination therapies to address multiple health concerns
By consulting with your physician and developing a personalized medication plan, you can ensure that your high blood pressure treatment is optimized for your unique needs.
Maximizing Medication Effectiveness
When it comes to managing high blood pressure, taking medication at the right time can make a significant difference. In this section, we'll explore the importance of consistency, monitoring, and lifestyle changes to maximize medication effectiveness.
Consistency is Key: Take Medication at the Same Time Every Day
Taking your high blood pressure medication at the same time every day is crucial for maintaining consistent blood pressure levels. This helps regulate your body's internal clock and ensures the medication is working effectively throughout the day. Aim to take your medication at the same time each day, such as with breakfast or before bed.
Monitor Blood Pressure Regularly to Adjust Medication Timing as Needed
Regular blood pressure monitoring is essential to understand how your medication is working. By tracking your blood pressure levels, you can identify patterns and adjust your medication timing accordingly. For example, if you find your blood pressure is higher in the morning, taking your medication at bedtime may be more effective. Work with your healthcare provider to determine the best monitoring schedule for you.
Lifestyle Changes, such as Diet and Exercise, Complement Medication
While medication is essential for managing high blood pressure, lifestyle changes can significantly complement its effectiveness. A balanced diet low in sodium, saturated fats, and added sugars, combined with regular physical activity, can help lower blood pressure levels. Aim for at least 30 minutes of moderate-intensity exercise, such as brisk walking, most days of the week. Additionally, stress-reducing activities like meditation or deep breathing exercises can also help manage blood pressure.
Conclusion: Tailoring Medication to Your Rhythm
When it comes to managing high blood pressure, timing is everything. Recent studies have shown that taking hypertension medication at bedtime may offer improved blood pressure control and reduced cardiovascular risk. This approach aligns with our natural circadian rhythm, allowing the body to respond more effectively to treatment.
Personalized Approaches to Hypertension Management
While bedtime medication may be beneficial for some, it's essential to consult your physician to determine the best medication timing for your unique needs. Factors such as lifestyle, sleep patterns, and individual health profiles can influence the effectiveness of treatment. A personalized approach to hypertension management can help optimize results and minimize potential side effects.
Customizing Treatment for Enhanced Outcomes
By working closely with your healthcare provider, you can develop a tailored treatment plan that suits your rhythm and lifestyle. This collaborative approach enables you to take a proactive role in managing your hypertension, leading to enhanced outcomes and improved overall well-being.










Comments ()