Migraine and Vision - When Eyes Play Tricks

Imagine waking up to a world that's distorted, like looking through a funhouse mirror – wavy lines, blind spots, and all. For millions, this isn't just a quirky optical illusion, it's a migraine warning sign. Vision symptoms can be a migraine's calling card, affecting nearly 1 in 5 people who suffer from these debilitating headaches. With growing research linking migraines to visual triggers and ocular symptoms, understanding this complex link is crucial for relief. Let's explore how migraines hijack our vision and what you can do to stop the distortion.
The Silent Suffering
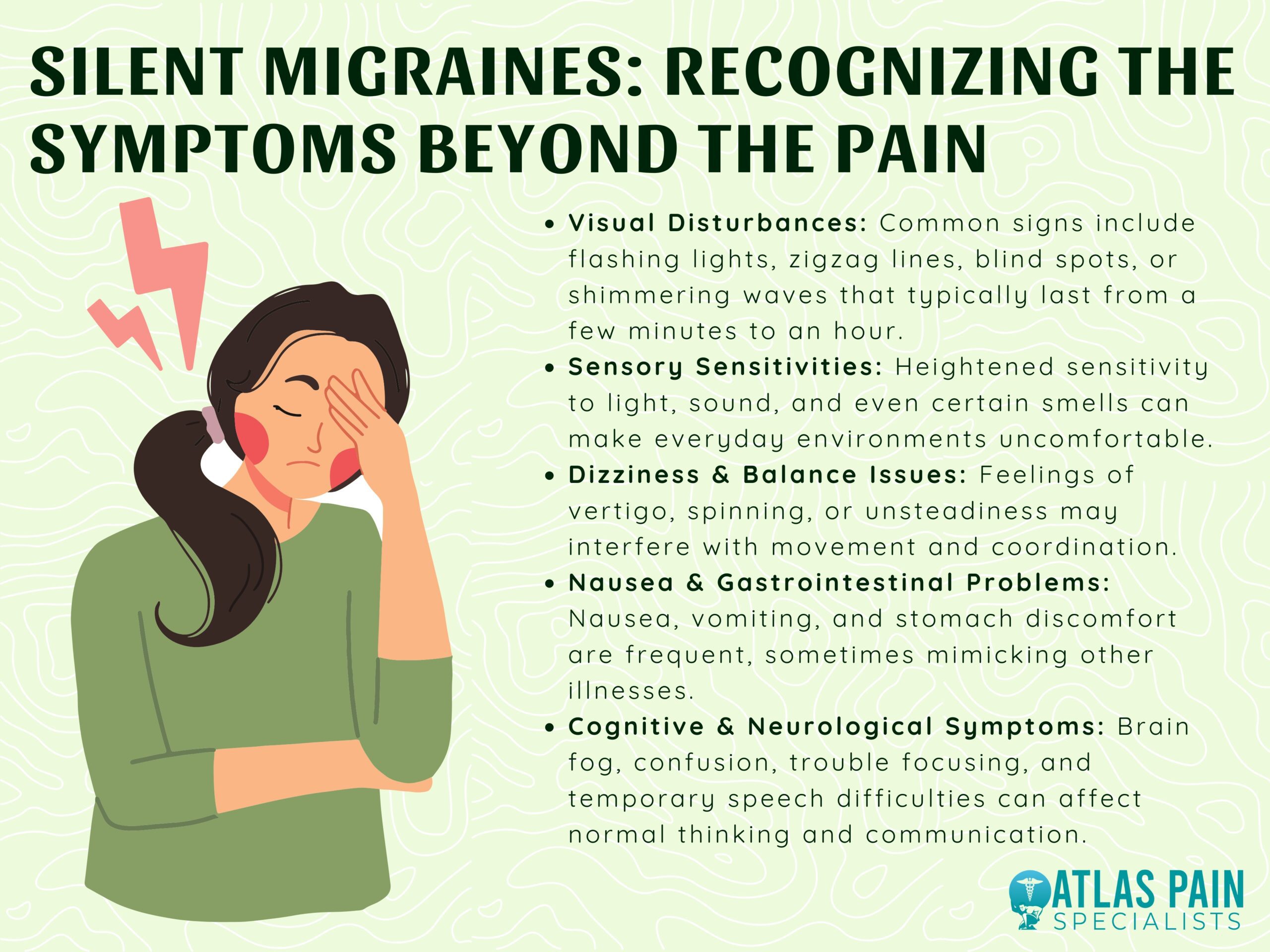
You might've heard of migraines, but do you know the real impact they have on millions of people? Migraine is the second leading cause of disability worldwide, affecting over 1 billion people globally, with 39 million Americans experiencing these debilitating episodes. That's a staggering number, isn't it?
The thing is, migraines aren't just about head pain. They're a complex neurological condition that can mess with your senses, making you super sensitive to light and sound. Imagine being in a crowded space with loud music and bright lights – it's like your brain is on overload!
Women are disproportionately affected, with research showing they're three times more likely to experience migraines than men. According to Dr. Kathleen Digre, a neurologist at the University of Utah, hormonal fluctuations play a significant role in this disparity.
Symptoms can vary widely, but common experiences include throbbing pain, nausea, and aura – which brings us to the fascinating connection between migraines and vision...
Decoding the Aura
You've probably heard of the term "aura" thrown around when people talk about migraines. But what does it really mean? For about 25% of people who experience migraines, the aura phase is a warning sign that a headache is on its way. It's like your brain's way of saying, "Hey, get ready, something's coming!"
Visual disturbances are a hallmark of aura symptoms. You're looking at things normally, and then suddenly, zigzag patterns start appearing – like someone's drawn a wiggly line across your field of vision. Some people see flashing lights, while others experience blind spots. Take Sarah, a 32-year-old graphic designer who experiences migraines with aura. She describes it as "like looking through a kaleidoscope, but only in one eye."
What to Expect
Aura symptoms typically don't last long – usually 20-60 minutes before the headache pain kicks in. During this time, some people might feel disoriented or have trouble finding words. Others might experience sensory changes, like tingling in their hands or face. These symptoms are usually temporary and resolve on their own once the headache starts.
- Zigzag patterns (fortification spectra)
- Blind spots (scotomas)
- Flashing lights (photopsia)
- Geometric shapes or patterns
Understanding your aura symptoms can help you prepare for the headache that's coming. Some people use this time to take medication or find a quiet space to ride it out. Dr. Peter Goadsby, a renowned migraine expert, says, "Recognizing aura symptoms can be a game-changer for people who experience migraines." By decoding your aura, you're taking back control of your migraines.
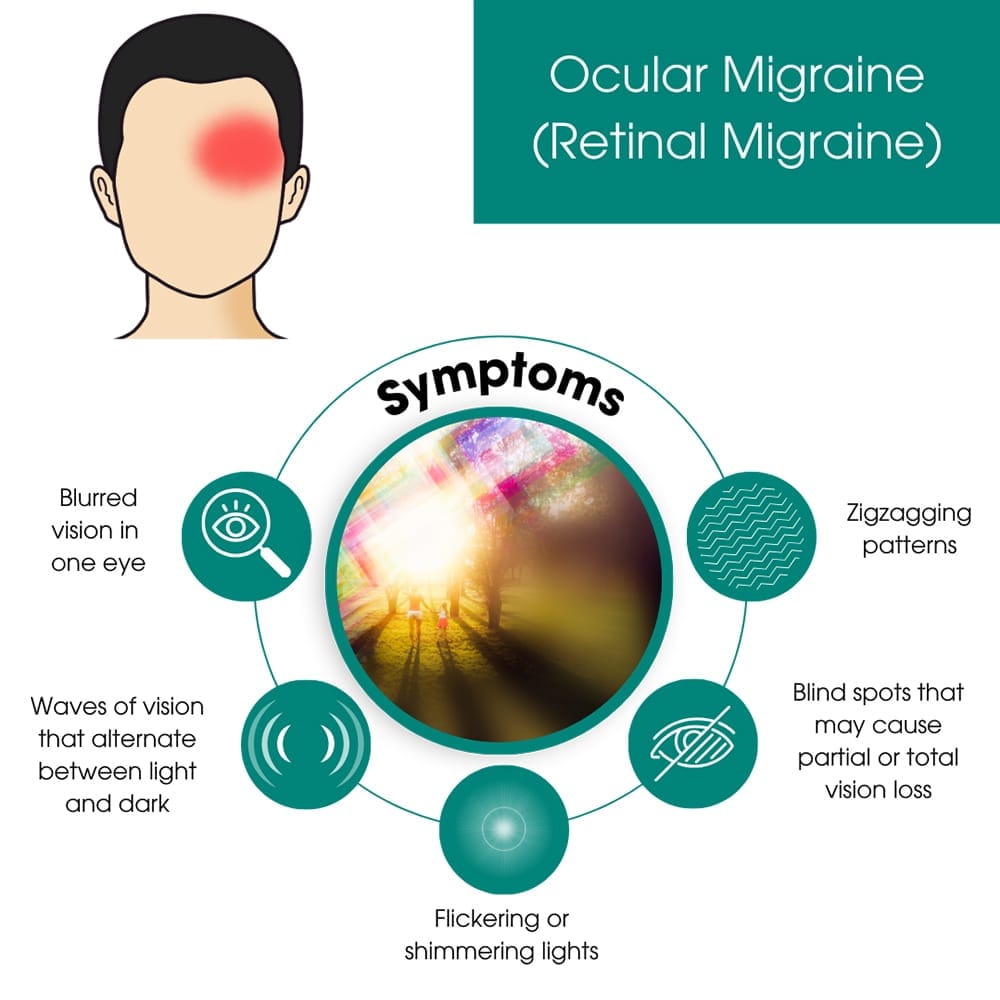
Ocular Migraine: Fact vs Fiction
You've probably heard of ocular migraines, but what exactly are they? Simply put, ocular migraines refer to visual disturbances that can be pretty unsettling. They're often characterized by zigzag patterns, blind spots, or flashing lights, and here's the kicker - they often occur without any head pain at all!
Take Sarah, a 32-year-old graphic designer who experienced an ocular migraine while working on a tight deadline. She described seeing shimmering lights that gradually expanded and then disappeared after about 20 minutes. Stress and hormonal changes are common triggers, and in Sarah's case, it was likely a combination of both. These migraines can be triggered by various factors, including stress, hormonal fluctuations, and even certain foods.
What to Expect
If you're experiencing an ocular migraine, here's what you can expect: symptoms usually resolve on their own within 30 minutes. That's right, 30 minutes - it might feel like an eternity, but trust me, it'll pass. During an episode, try to find a quiet spot, dim the lights, and take slow, deep breaths. Some people find relief with a cold compress or a cup of ginger tea.
- Visual disturbances can last anywhere from a few minutes to an hour
- Symptoms can be alarming, but they're usually harmless
- Ocular migraines can be a sign of an underlying condition, so it's essential to consult a doctor if you're experiencing them frequently
While ocular migraines can be unsettling, understanding what they are and what triggers them can help you prepare and manage them better. If you're experiencing frequent or severe episodes, don't hesitate to reach out to a healthcare professional for guidance.
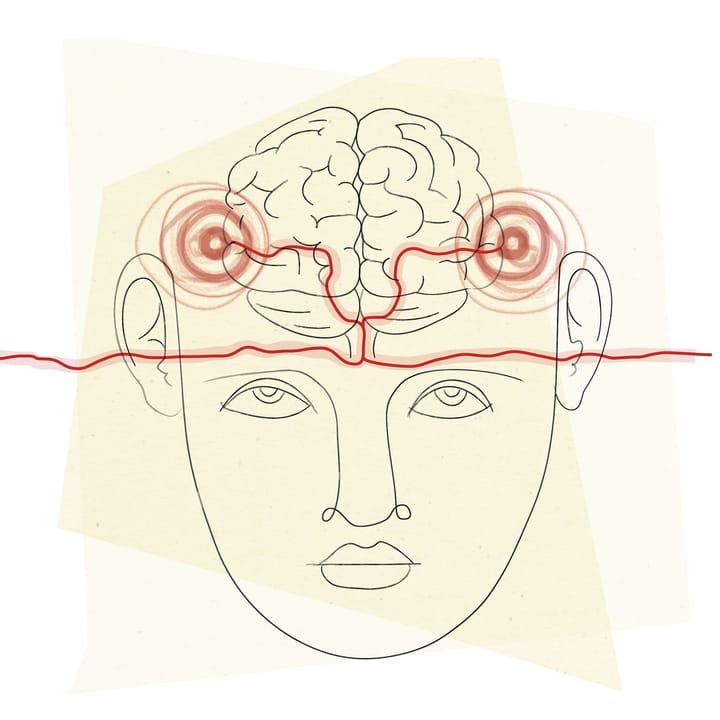
The Brain-Eye Connection
You're probably familiar with the idea that your brain processes visual information. But when it comes to migraines, this connection gets really interesting. Research suggests that migraines might be triggered by abnormal brain activity that affects the visual pathways. This can cause a range of visual symptoms, from flashing lights to blind spots. Let's dive deeper into this connection. Studies have shown that certain areas of the brain, like the visual cortex, are more active in people who experience migraines with aura (that's the fancy term for visual symptoms). For example, a study published in the journal Neurology found that people with migraines showed increased activity in the visual cortex, even between attacks. Visual triggers can also play a significant role in triggering migraine attacks. You might have noticed that certain things can set you off - bright lights, patterns, or even scrolling through your phone for too long. You're not alone. Research suggests that up to 90% of people with migraines have some kind of visual trigger. For instance, Dr. David Welch, a migraine specialist, notes that "some people are particularly sensitive to certain types of light, like fluorescent lighting or high-contrast patterns." Some people experience persistent visual symptoms between migraine episodes, a phenomenon known as persistent aura without infarction. This can be quite disconcerting, especially if you're not expecting it. For example, a patient of Dr. Welch's reported seeing shimmering lights and zigzag patterns for hours after her migraine had resolved.
What does this mean for you?
Understanding the brain-eye connection can help you better manage your migraines. By identifying your visual triggers and taking steps to avoid them, you might be able to reduce the frequency and severity of your attacks. This could involve simple changes like wearing tinted glasses, adjusting your screen settings, or practicing relaxation techniques. You might be wondering what you can do to identify your visual triggers. One way is to keep a migraine diary, tracking when your attacks occur and what might have triggered them. This can help you spot patterns and correlations that you might not have noticed otherwise. Dive deeper: How can I identify my migraine triggers? What are some common visual triggers for migraines? Can relaxation techniques help with migraine management?
Diagnosis Challenges
So, you've been experiencing these weird vision issues, and you're wondering if it's just a migraine thing or something more serious. Here's the thing: diagnosing migraines can be super tricky. There's no single test that can confirm it, so doctors have to rely on your medical history and symptoms.
That's where criteria like frequency and duration come in. For instance, the International Headache Society says you've gotta have at least five headache attacks that last 4-72 hours, with symptoms like nausea, sensitivity to light, or vision issues. Dr. Anne MacGregor, a headache specialist, says, "A thorough medical history is crucial – it's like being a detective, piecing together the clues." Keeping a headache diary can really help with this. You can track when your headaches hit, how long they last, and what might've triggered them.
A Case in Point
Take Sarah, a 32-year-old teacher who'd been experiencing vision issues – zig-zag patterns, blind spots, the works. She thought it was just stress, but turns out she was having ocular migraines. Her doctor used her headache diary to identify patterns and triggers, and voilà! She got a proper diagnosis and treatment plan.
So, if you're experiencing weird vision symptoms, don't be afraid to track them and talk to a doc. It's all about understanding your own patterns and figuring out what's going on. And hey, if it is a migraine, there are treatments out there that can help.
- Headache frequency: at least 5 attacks
- Duration: 4-72 hours
- Symptoms: nausea, sensitivity to light, vision issues
Treatment Options
You're not alone if you're searching for relief from migraines that affect your vision. The good news is that there are several treatment options available, and what works best often depends on the severity and frequency of your migraines.
Medications for Quick Relief
Triptans are a popular choice for treating migraines, and they're most effective when taken early. These medications work by constricting blood vessels and blocking pain pathways in the brain. For example, sumatriptan (Imitrex) is a commonly prescribed triptan that can provide relief within two hours for many people. Your doctor might also recommend anti-nausea meds or pain relievers like ibuprofen or acetaminophen.
Lifestyle Changes to Reduce Frequency
Making a few simple changes to your daily routine can make a big difference. Stress management techniques like yoga, meditation, or deep breathing can help reduce migraine frequency. Getting enough sleep is also crucial – aim for 7-8 hours per night. Keeping a headache diary can help you identify triggers, whether it's certain foods, hormonal changes, or sensory stimuli.
Options for Chronic Sufferers
If you're experiencing migraines frequently, Botox injections or nerve blocks might be worth exploring. Botox has been shown to reduce migraine frequency by targeting specific pressure points. Nerve blocks, on the other hand, involve injecting anesthetics or steroids into specific nerves to block pain signals. These treatments can be effective for people who haven't responded well to other options.
- Stress management techniques (yoga, meditation, deep breathing)
- Sleep hygiene (7-8 hours per night)
- Avoiding triggers (certain foods, hormonal changes, sensory stimuli)
- Botox injections
- Nerve blocks
Living with Migraine
If you're one of the millions dealing with chronic migraines, you know how isolating it can feel. But here's the thing: you're not alone. Support groups, both online and in-person, can be a game-changer. Take the Migraine Support Group of India, for example, which has over 10,000 members sharing their experiences and advice on managing symptoms.
Alternative Relief
Some people find relief through alternative therapies like acupuncture and biofeedback. Acupuncture, in particular, has shown promise in reducing migraine frequency and severity. A study published in the Journal of Traditional Medicine found that patients who received acupuncture had a 50% reduction in migraine attacks. Biofeedback, on the other hand, helps you tune into your body's signals, allowing you to control physical responses that might trigger a migraine.
Tracking your triggers and symptoms is also key. Apps like Migraine Buddy and My Migraine Tracker let you log your symptoms, triggers, and medication, giving you a clear picture of your patterns. This data can be super valuable when working with your doctor to tailor a treatment plan that's right for you.
For instance, Sarah, a 32-year-old marketing executive, was able to reduce her migraines by 70% simply by tracking her symptoms and identifying her triggers – in her case, stress and certain foods. With this knowledge, she was able to make lifestyle changes and work with her doctor to develop a personalized treatment plan.
- Identify your triggers
- Track your symptoms
- Explore alternative therapies
- Join a support group
The bottom line? There's no one-size-fits-all solution, but with the right tools and support, you can take control of your migraines.
Hope on the Horizon
You've made it this far, and there's exciting news ahead! Researchers are working tirelessly to tackle migraines, and new treatments are being developed as you read this. We're talking about therapies targeting specific pathways like CGRP (calcitonin gene-related peptide), which has already led to breakthroughs with medications like Aimovig and Emgality.
Personalized Relief is Coming
The future of migraine management is looking increasingly personalized. Doctors are honing in on individual symptoms and triggers, crafting tailored plans to tackle the condition head-on. For instance, studies have shown that identifying and avoiding specific triggers can reduce migraine frequency by up to 50% in some people.
- New CGRP-targeting medications offer hope for frequent sufferers
- Personalized treatment plans are yielding promising results
- Ongoing research aims to unlock further mysteries of the brain
We're on the cusp of a new era in migraine management, where understanding the intricacies of your brain's wiring could be the key to unlocking a life with fewer headaches. By staying informed and working closely with healthcare providers, you're positioning yourself to benefit from these advancements.
The bottom line? There's never been a more promising time for those living with migraines. Hang in there – relief is being researched, developed, and approved as we speak. Imagine a future where migraines no longer dictate your day-to-day life. That's the hope we're holding onto.












Comments ()