Inflammatory Bowel Disease - Uncovering the Hidden Triggers
The Mysterious Causes of Inflammatory Bowel Disease
Imagine having a war waging inside your gut, with no clear enemy in sight. That's what it can feel like to live with Inflammatory Bowel Disease (IBD). Despite affecting millions of people worldwide, the exact cause of IBD remains a mystery, but researchers are getting closer to uncovering the hidden triggers.
So, what's thought to be behind this debilitating condition? Research suggests that an abnormal immune response to the gut microbiome may play a significant role in developing IBD. Think of it like an overzealous security guard who mistakes friendly gut bacteria for intruders, triggering an all-out attack on the digestive tract.
Genetic and Environmental Factors
Genetic markers can predispose some people to IBD. For instance, studies have shown that individuals with a family history of IBD are more likely to develop the condition. But genes aren't the only culprit. Environmental factors, such as being raised in a sterile environment or taking antibiotics during the first year of life, may also contribute to the development of IBD.
Some interesting stats highlight the potential role of environmental factors:
- Children who receive antibiotics in their first year of life are 2.9 times more likely to develop IBD.
- People living in urban areas are more likely to develop IBD than those in rural areas.
While we can't pinpoint a single cause, understanding these potential triggers can help researchers develop more effective treatments and maybe, just maybe, prevent IBD from taking hold in the first place.
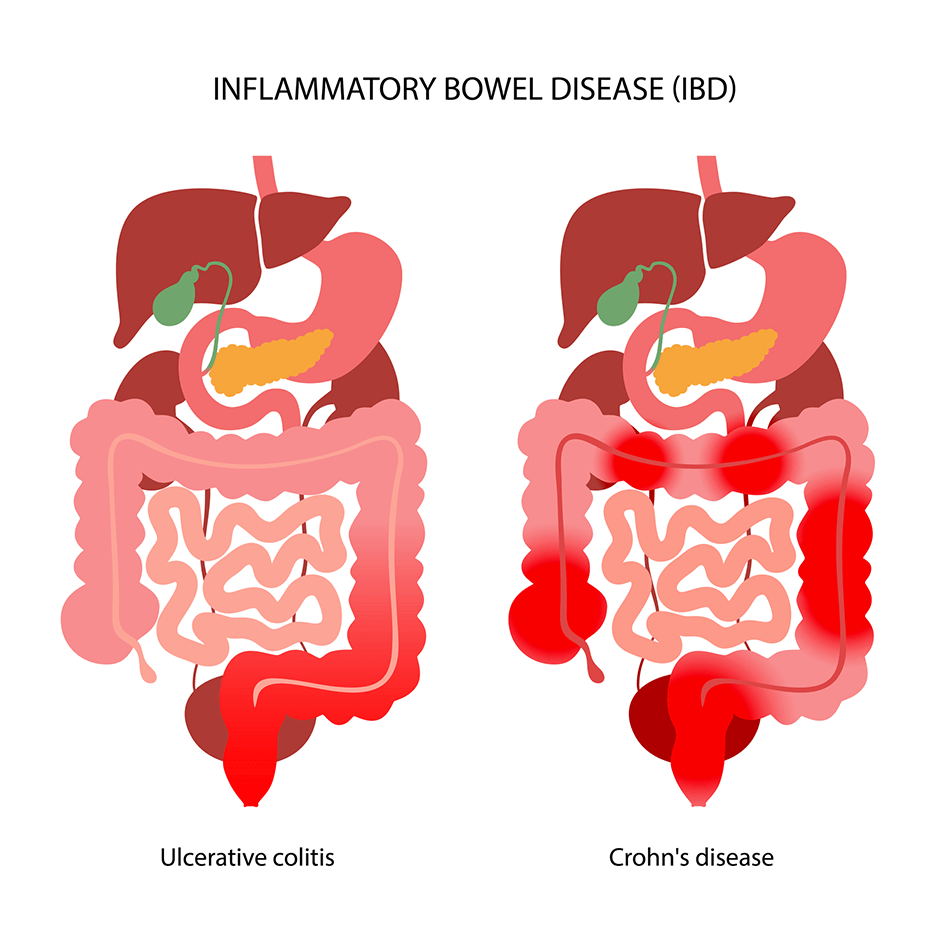
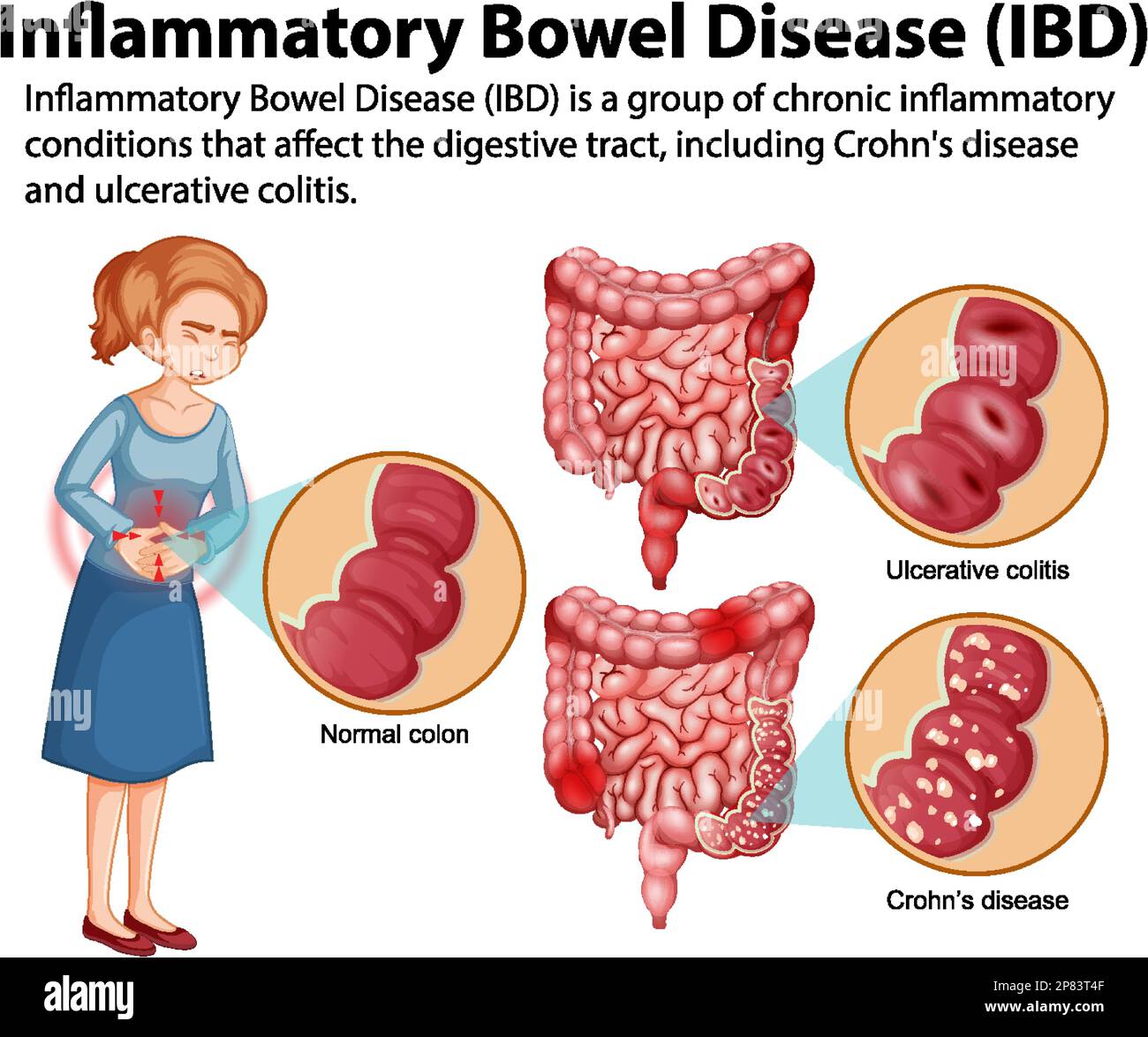
The Two Main Types of IBD: Crohn's and Ulcerative Colitis
Imagine having a constant, unwelcome companion in your gut - one that brings pain, discomfort, and uncertainty to your daily life. For millions of people worldwide, this is a harsh reality due to Inflammatory Bowel Disease (IBD). Let's dive into the two main culprits behind this misery: Crohn's disease and ulcerative colitis.
Crohn's Disease: The Whole Gut Troublemaker
Crohn's disease is like a troublemaker that can affect any part of your digestive tract, from your mouth to your, ahem, exit. But it loves to hang out in the small intestine, causing inflammation and damage that can lead to symptoms like persistent diarrhea, belly pain, and weight loss. About 780,000 people in the US are living with Crohn's, and it's often diagnosed in people in their teens and early twenties.
Ulcerative Colitis: The Colon's Nemesis
Ulcerative colitis, on the other hand, is more of a specialist - it primarily targets the colon and rectum, causing inflammation and sores in the digestive tract. Symptoms can range from mild to severe and include bloody stools, abdominal pain, and a sudden urge to go to the bathroom. According to the Crohn's & Colitis Foundation, about 907,000 people in the US are living with ulcerative colitis.
Both Crohn's and ulcerative colitis can significantly impact daily life, causing emotional distress and social anxiety. If left untreated, these conditions can lead to complications like narrowing of the intestine, bowel obstruction, and even cancer. Treatment options vary depending on the severity and extent of the disease, but medications, lifestyle changes, and surgery are common approaches.
Risk Factors: Who's More Likely to Develop IBD?

When it comes to Inflammatory Bowel Disease (IBD), figuring out who's most at risk can feel like trying to solve a puzzle. But researchers have been working hard to uncover the pieces, and some patterns are starting to emerge.
Age is one big factor. Most people are diagnosed with IBD before they hit 30, with the peak age range typically falling between 15 and 25 years old. This is a time when life is already pretty chaotic – high school, college, early careers – and dealing with chronic illness might be the last thing on your mind.
Family Ties
Family history also plays a significant role in determining your risk. If you've got a blood relative with IBD, you're more likely to develop it too. In fact, studies suggest that if one parent has IBD, their child is 2-13 times more likely to develop the condition. That's a pretty significant increase.
Lifestyle Factors
But here's the good news: some risk factors you can control. Cigarette smoking, for example, is the most significant controllable risk factor for developing Crohn's disease. Smokers are more than twice as likely to develop Crohn's as non-smokers. Quitting smoking can significantly reduce your risk – and your doctor will be the first to encourage you to kick the habit.
Other potential risk factors include:
- Genetic predisposition
- Imbalance of gut bacteria
- Certain medications
Understanding these risk factors can help you take proactive steps to reduce your chances of developing IBD. While there's no guaranteed way to prevent it, knowing what you're up against can make all the difference.
Complications of IBD: The Domino Effect
Imagine dealing with a never-ending storm in your gut, where every meal can trigger a painful reaction and every trip to the bathroom is a gamble. That's the reality for millions living with Inflammatory Bowel Disease (IBD). But the trouble doesn't always stop there - IBD can set off a chain reaction of complications that affect not just your digestive system, but your overall health.
Beyond Gut Feelings: Systemic Complications
IBD increases the risk of developing colon cancer, with studies suggesting that people with ulcerative colitis are at a 2-3 times higher risk compared to the general population. Skin issues like psoriasis and erythema nodosum can also crop up, affecting up to 15% of people with Crohn's disease. Then there are the eyes - uveitis, a form of eye inflammation, can cause blurred vision and even blindness if left untreated. Joint inflammation, or arthritis, is another common companion, impacting around 30% of people with IBD.
One of the most concerning complications is primary sclerosing cholangitis (PSC), a disease that scars and narrows the bile ducts. About 70-80% of people with PSC also have IBD, and it can lead to liver damage and even liver failure.
Condition-Specific Complications
- Crohn's disease: bowel obstruction, malnutrition, and fistulas
- Ulcerative colitis: toxic megacolon and perforated colon
These complications can be severe and require immediate medical attention. Bowel obstruction, for instance, can cause severe abdominal pain, vomiting, and constipation. Fistulas, abnormal connections between the intestine and other organs or the skin, can lead to infections and abscesses. Toxic megacolon, a rare but life-threatening complication of ulcerative colitis, can cause the colon to expand and potentially rupture.
Understanding these potential complications is crucial for managing IBD effectively. By knowing what to watch out for, you can work with your healthcare team to prevent or minimize these issues and improve your overall quality of life.
Living with IBD: Managing the Symptoms

Imagine having a persistent stomach ache that just won't quit, or feeling like you're stuck to the bathroom. For people living with Inflammatory Bowel Disease (IBD), these symptoms are all too real. While there's no cure for IBD, there are ways to manage the symptoms and induce remission.
Finding the Right Treatment Plan
Medications are often the first line of defense against IBD symptoms. Aminosalicylates, corticosteroids, and immunomodulators can help reduce inflammation and manage symptoms. For example, studies have shown that 50-70% of people with Crohn's disease achieve remission with azathioprine treatment. But medication isn't the only piece of the puzzle.
Lifestyle changes can also make a big difference. Stress management techniques like meditation, yoga, or deep breathing can help reduce stress and alleviate symptoms. Getting regular exercise, quitting smoking, and staying hydrated can also help manage symptoms.
Dietary Modifications
Food can be a trigger for IBD symptoms, but don't worry, you're not doomed to a life of bland salads. Identifying and avoiding trigger foods can help alleviate symptoms. Some common culprits include:
- Dairy products
- High-fiber foods
- Spicy or fatty foods
Working with a registered dietitian or healthcare professional can help you develop a personalized diet plan that works for you. For example, some people find that a low-FODMAP diet helps reduce symptoms like bloating and abdominal pain.
The key is to work with your healthcare team to develop a treatment plan that's tailored to your needs. With the right combination of medication, lifestyle changes, and dietary modifications, it's possible to manage symptoms and improve quality of life.









Comments ()